Understanding Medicare
What is Medicare?
Medicare is a federally funded health insurance program that provides health care benefits to people 65 years and older, younger people with certain disabilities, and people of any age who have permanent kidney failure or end-stage renal disease (ESRD) and require dialysis or a kidney transplant.
Learn the parts of Medicare
The ABCs of Medicare
What is Medicare supplemental insurance or a Medigap policy?
What is a Medicare Advantage plan?
Medicare Advantage plans are a way for people eligible for Medicare to get coverage for health care services. Medicare Advantage plans are regulated by the Centers for Medicare & Medicaid Services and offer all benefits covered by Original Medicare.
While Original Medicare allows people with Medicare to visit any health care facility and see any doctor who accepts Medicare, Medicare Advantage plans have a network of providers and hospitals that members can use.
The ABCs of Medicare
There are four basic parts of Medicare: A, B, C and D. Each part helps pay for certain health care services. Each part also has certain costs that you may have to pay. Your Medicare costs will depend on what coverage you choose and on what health care services you use.
Peoples Health plans are Part C, Medicare Advantage plans, which require that our members are entitled to Medicare Part A and enrolled in Medicare Part B. Most Peoples Health plans also include Part D prescription drug coverage.

Part A – Hospital Insurance
Part A hospital insurance covers inpatient hospital services, blood, skilled nursing facility care, home health and hospice care. Most people do not pay a premium for Part A services. For some services (for example, inpatient hospital stays), they will need to pay a deductible before Medicare coverage begins. The deductible amount may change from year to year.
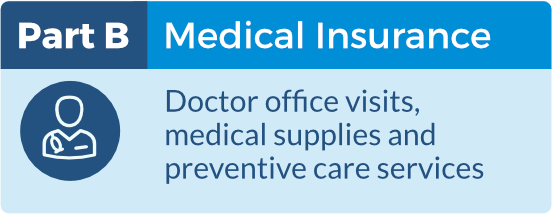
Part B – Medical Insurance
Part B medical insurance covers doctor, outpatient hospital, home health and preventive services, as well as other services Part A does not cover. You can choose if you want to enroll in Part B. Most people must pay a monthly premium to receive coverage. (This premium may be paid by an organization on your behalf.) The premium amount may change from year to year and is based on annual income.
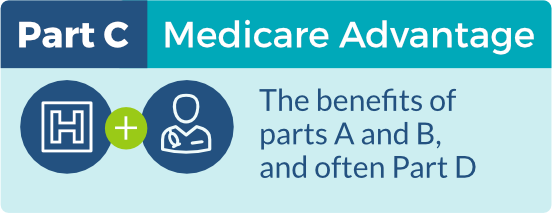
Part C – Medicare Advantage
Part C Medicare Advantage plans are paid by Medicare to provide health care coverage to people with Medicare. These plans must offer all benefits that Original Medicare offers, plus Medicare Advantage plans can provide extra benefits and lower your out-of-pocket costs. Most Medicare Advantage plans also include Part D prescription drug coverage. To join a Part C Medicare Advantage plan, you must be enrolled in Medicare parts A and B.
Peoples Health is a Medicare Advantage organization that offers Medicare Advantage plans. Click here to learn more about Medicare Advantage plans and how they work.
Part D – Drug Coverage
Part D outpatient prescription drug coverage is optional coverage provided by private health insurance plans that have a contract with Medicare. Part D covers prescription drug costs and can be received through a stand-alone prescription drug plan or through a Medicare Advantage prescription drug plan. Depending on the plan, there may be a premium for the Part D coverage.
The prescription drug coverage cycle
Phase 1
Yearly Deductible Stage
For plans with a drug deductible, the beneficiary begins in Phase 1 (Yearly Deductible Stage). During this stage, the beneficiary must pay the full cost of some or all their drugs until they reach the plan’s deductible amount. Once the beneficiary meets the deductible, they leave the Deductible Stage and move to Phase 2.
Phase 2
Initial Coverage Stage
During Phase 2 (Initial Coverage Stage), the beneficiary pays the standard plan cost for each drug, and the plan pays the rest of the cost. The beneficiary stays in this stage until their total out-of-pocket drug costs (the amount paid by the beneficiary or others on their behalf) reach an amount specified by Medicare. This amount may change from year to year.
Phase 3
Catastrophic Coverage Stage
During the final phase, Phase 3 (Catastrophic Coverage Stage), the plan pays most or all costs for covered drugs, and the beneficiary pays no or reduced costs.
Phase 1
For plans with a drug deductible, the beneficiary begins in Phase 1 (Yearly Deductible Stage). During this stage, the beneficiary must pay the full cost of some or all their drugs until they reach the plan’s deductible amount. Once the beneficiary meets the deductible, they leave the Deductible Stage and move on to phase 2.
Phase 2
During Phase 2 (Initial Coverage Stage), the beneficiary pays the standard plan cost for each drug, and the plan pays the rest of the cost. The beneficiary stays in this stage until his or her total drug costs (the amount paid by both the beneficiary and his or her plan) reach an amount specified by Medicare. This amount may change from year to year.
Phase 3
During Phase 3 (Coverage Gap Stage), the beneficiary pays higher costs for many or all drugs. However, the Medicare Coverage Gap Discount Program provides a discount on the cost for most brand-name drugs. The amount of the discount may change each year. Some plans may provide additional coverage for beneficiaries during the coverage gap stage. The beneficiary stays in the coverage gap stage until his or her total out-of-pocket drug costs (the amount the beneficiary pays and the amount paid by others on the beneficiary’s behalf) reach an amount specified by Medicare. This amount may change from year to year. The amounts paid by others on the beneficiary’s behalf may include drug assistance programs like the Extra Help program, and it also may include amounts paid by organizations like the U.S. Department of Veterans Affairs or the Medicare Coverage Gap Discount Program. The beneficiary then moves into phase 4.
Phase 4
During the final phase, Phase 4 (Catastrophic Coverage Stage), the plan pays most or all of the costs for covered drugs, and the beneficiary pays reduced costs.

What is Medicare supplemental insurance or a Medigap policy?
Supplemental insurance helps fill in the “gaps” for medical care that may not be covered by Medicare. It helps with costs for coinsurance, copays and deductibles. There is usually an additional premium that must be paid for supplemental insurance.